Referring Physician Information on ABUS Supplemental Breast Cancer Screening
The topic of breast density has grown in importance, and management of patients with dense breast tissue is of concern. South Carolina mandates that after a mammogram, patients receive a results letter that includes information about their breast density.
In addition, they will be told that supplemental screening may be beneficial and they should talk to their physician. Below is a video and background information on Automated Breast Ultrasound (ABUS) – a new screening tool available at the Beaufort Memorial Breast Health Center.
Unlike screening mammography, a physician's order is required for supplemental ultrasound screening.
Patients may ask you about the additional screening and whether it is covered by their insurance. To determine coverage, they should contact their insurance provider and provide the CPT code 76641: Ultrasound, breast, unilateral, real time with image documentation, including axilla when performed; complete.
You can use this material to help inform your patients about what it means to have dense breasts, supplemental screening options and insurance coverage for the additional screening.
Facts About Dense Breasts
Many patients do not understand what it means to have “dense breasts.” Physicians need to understand both the risks associated with dense breasts and be informed about supplemental screening benefits and options.
Here are the facts:
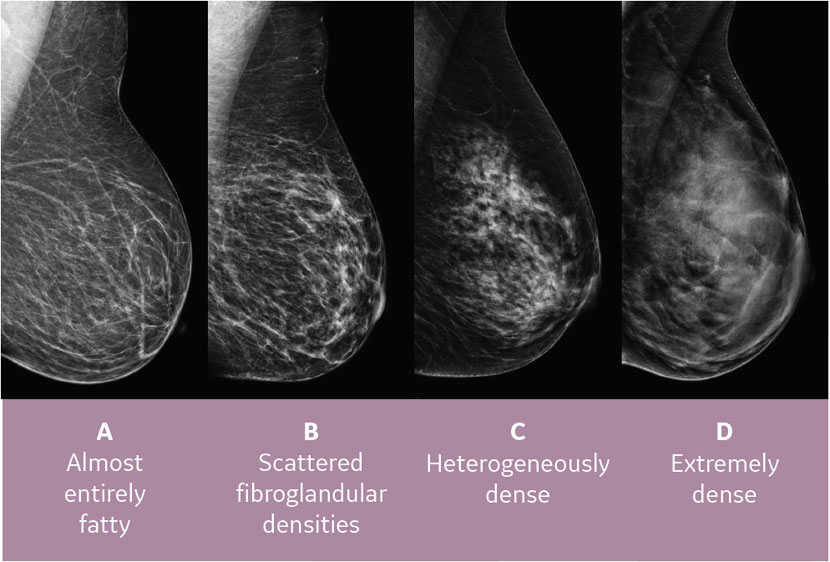 “Density” is an indicator of how much connective tissue relative to the fatty tissue is in the breast. This image shows the four categories of “density.”
“Density” is an indicator of how much connective tissue relative to the fatty tissue is in the breast. This image shows the four categories of “density.”- Mammography displays both dense tissue and masses as white, making masses harder to detect. Supplemental screening, such as ultrasound, helps uncover masses that may be obscured in dense tissue.
- Over 40% of American women aged 40 to 74 years have dense breasts.1 It is very common and normal.
- The Journal of the American Medical Association (JAMA) recently published a study that concluded breast density was the most common risk factor for breast cancer.2
- Dense breast tissue increases the likelihood of developing cancer 4-6 times, compared to having non-dense breasts.3
Supplemental Screening Options for Dense Breasts
- According to the American Cancer Society, women with dense breasts may benefit from supplemental imaging tests such as Breast Ultrasound or MRI.
- The American College of Radiology recommends the following:
- Average to low risk women with dense breasts: ultrasound
- High risk with dense breasts: MRI
Ultrasound and MRI may be able to detect additional cancer that would not be seen on a mammogram. If cancer is diagnosed at an earlier stage, it lowers the need for more aggressive treatments like surgery and chemotherapy.4
Automated Breast Ultrasound (ABUS) Supplemental Screening
The Invenia™ ABUS 2.0 is the only ultrasound technology FDA approved for screening women with dense breasts. When used in addition to mammography, Invenia ABUS 2.0 can improve breast cancer detection by 37.5 percent over mammography alone.5
- ABUS can detect more cancers over mammography alone5
- It is relatively low cost
- There is no radiation
Will health insurance pay for supplemental screening like they do mammograms? What do I tell my patients?
Insurance may pay for the supplemental screening, but patients should check with their individual plan. Because this is supplemental screening, it may be applied to their deductible or include a co-pay like other examinations. Patients can speak with our schedulers and get the CPT code so they can ask their insurance company about coverage.
It is important to note over 38 states have enacted dense breast notification laws (as of October 2019). This has resulted in an increase in the use of supplemental ultrasound and improved cancer detection.6
Commonly Asked Questions From Patients
1. My screening mammogram was covered 100% – will my ultrasound be?
Your insurance company pays for the cost of “screening” tests like mammography, which is considered under preventative and wellness programs. The ultrasound would be considered a supplemental screening test and may be subject to your deductible and co-pay. Contact your insurance provider and provide the CPT code (76641: Ultrasound, breast, unilateral, real time with image documentation, including axilla when performed; complete) to confirm coverage.
2. Does South Carolina mandate insurance coverage for supplemental screening?
As of July 2020, South Carolina does not mandate coverage. This does not mean that all insurers will not cover additional screening. Plans that do include coverage may still require a co-pay and/or be subject to a deductible. Call your insurance company to confirm your coverage to avoid unexpected costs.
3. Since South Carolina does not mandate coverage, how will I know if my insurance company will cover it?
Most insurance companies will cover the supplemental screening,7 but it is best to call and ask in advance.
Beaufort Memorial has partnered with MDsave to offer discounted package pricing on mammograms and supplemental ultrasound screening. If you do not have coverage or a high deductible, an MDsave voucher could save you money.
4. Will I have a deductible or co-pay?
This will depend on your individual insurance plan. Magellan8 recently reviewed claims data and the average out-of-pocket cost across the country was $52 (ranging from $3-$351).
5. How do I find out what my insurance company will cover and pay?
- Call your insurance company and tell them you have been notified you have dense breasts and your physician is recommending a supplemental screening ultrasound.
- Tell your insurance company that the procedure code or CPT code is 76641: Ultrasound, breast, unilateral, real time with image documentation, including axilla when performed; complete.
- Ask them if they will cover the cost of the exam. Also ask if you will have an out-of-pocket cost.
6. What do I do if the exam is not covered?
- Ultrasound exams, like ABUS, are usually a covered procedure; however in some states, it is not covered under the Affordable Care Act as a screening procedure (like your screening mammogram). It may be subject to your deductible and/or you would have an out-of-pocket expense/co-pay.
- Should it be denied, ask your healthcare provider to file an appeal.
- If you do not want it to be subject to your deductible, you may ask Breast Health Center scheduling staff at 843-522-5015 if there is an option for an out-of-pocket cash price.
It is important that your patients understand their overall risk for breast cancer, if they have dense breasts, and that you speak to them about supplemental screening options. Like most other tests, supplemental screening may require a co-pay and/or be subject to a patient’s deductible, but it is recommended patients talk with their insurance company in advance of scheduling to avoid any unexpected fees.
References:
- Sprague BL, Gangnon RE, Burt V, Trentham-Dietz A, Hampton JM, Wellman RD, et al. Prevalence of mammographically dense breasts in the United States. J Natl Cancer Inst. 2014;106. [PMID: 25217577] doi:10.1093/jnci/dju255.
- Engmann NJ, Golmakani MK, Miglioretti DL, et. Al Population-Attributable Risk Proportion of Clinical Risk Factors for Breast Cancer. JAMA Oncol. 2017 Sep 1; 3(9):1228-1236.
- Boyd, et al, NEJM Jan 2007.
- Sparano, JA, et al. N Engl J Med 2018; 379:111-121.
- FDA PMA P110006 summary of safety and effectiveness.
- Busch, SH, Hoag, JR, Aminawung JA, et al. Association of State Dense Breast Notification Laws with Supplemental Testing and Cancer Detection After Screening Mammography. AJPH May 2019 Vol. 109, No. 5.
- Review of ABUS coverage via Canary Insights, a data base of 270 commercial and Medicare payers. Coverage review as of May 2019. Data on file with Emerson.
- Magellan claims review. Commercial Reimbursement and Utilization for Invenia ABUS (Automated Breast Ultrasound) www.gehealthcare.com/inveniaabus.
